There are two sides to every surgery. Evaluate the perspective of a patient versus a surgeon as they discuss how compassionate care and innovative technology lead to better outcomes.

Surgery will never be “fun,” but its goal is to create a better quality of life. Through compassionate care and innovative technology, surgeons are continuously saving and improving the lives of their patients.
Just ask Donna Haen, a patient who underwent surgery four times during 2017. Or ask Dr. Daniel J. Farrugia, a fellowship-trained breast surgeon who exudes empathy for patients and enthusiasm for new technology. Their stories champion the humanity inherent to surgery.
A Patient’s Perspective
Vaguely, Donna Haen remembers waking up around 1 a.m. on April 1, 2017. The pain in her stomach was too intense to ignore.
“Thank God I called my sister,” she says. “It’s a blur, but I remember her picking me up, and getting to the emergency room. I needed to get there fast and my daughter was out of town.”
With a history of stomach problems, it wasn’t unusual for Haen to feel uncomfortable; nausea had long ago become a part of her everyday life. But never before had things felt this bad.
The doctors at Presence Saint Joseph Hospital, in Elgin, immediately began to “run some tests.” The last thing Haen recalls is the sensation of nasogastric intubation, a process that involved the insertion of a plastic tube through her nose, past her throat, and down into her stomach.
“I remembered them trying to get the tube down, but it wasn’t working,” Haen says. “After that, I remember nothing.”
—
Dr. David Ryan, a general surgeon, was working on-call that night. As one of four physicians at Midwest Surgery, with locations in St. Charles and Elgin, he often sees patients at nearby hospitals. He calls his schedule “predictably unpredictable,” since he knows he could be needed at any moment during his on-call shifts.
As a general surgeon, he has a wide scope of knowledge. For the most part, he does abdominal surgeries – hernia repairs, appendectomies – but he also deals with colon cancer, gallbladder disease, a variety of skin cancer problems and other emergency cases.
For him, it’s routine to spring into action in the early morning hours when a patient is in need.
“I think people sometimes look at medicine, and particularly surgery, as a glamorous lifestyle where we think of ourselves as elitists. But, that’s certainly not typical of the average surgeon,” Ryan says.
“Oftentimes, outside of the United States, you’ll be seen in the morning regardless of the problem. So, while I certainly don’t enjoy getting up in the middle of the night, I do it because it’s what people need.”
When Ryan arrived at Presence Saint Joseph Hospital, Haen was already in critical condition. The pain that woke her during the night was due to gastrointestinal perforation, also known as a perforated bowel. A hole had developed somewhere in her digestive tract, and an emergency surgery was necessary.
—
The next thing Haen remembers is waking up in the Intensive Care Unit (ICU). She was shocked to learn the date and hear of the events that had transpired.
“My daughter was at my bedside and I said to her, ‘We’re supposed to be in Arizona,” and she told me ‘Mom, it’s April 5,’” Haen recalls.
Four days had passed since she initially arrived at the emergency room.
First, Haen learned she underwent an ileostomy procedure. Dr. Ryan had surgically created an opening (stoma) in her abdominal wall so that he could bring the end of her small intestine (ileum) onto the surface of her skin. This allowed for a pouch to collect her digested food.
But even more shocking, Haen learned that she also had a stroke while in the ICU.
“It all happened when I was in a coma,” she says. “I really lucked out, considering how strokes can affect people. I had to re-learn how to swallow, which wasn’t easy. But overall, I’m lucky the stroke happened in the left side of my brain so there wasn’t too much damage.”
Haen spent a month at Presence Saint Joseph Hospital, with 10 days total in the ICU. Over the next few months, she would end up seeing Dr. Ryan three more times for surgery. On July 20, 2017, he reversed her ileostomy during a scheduled procedure.
But in September, Haen had another emergency. And yet another in November.
“I had two bowel blockages, which I was at a high risk for, considering all of the stomach surgeries I’ve had in the past,” she says. “So, between the initial trip to the emergency room, the ileostomy reversal, and then the two bowel blockages, Dr. Ryan’s actually done surgery on me four times.”
The bowel blockages were caused by a buildup of scar tissue from Haen’s previous procedures. Once again, for both emergencies, she rushed to the hospital during the night.
“I’m very glad Dr. Ryan was always the person I saw,” Haen says. “He’s the one who ‘cleaned out’ my scar tissue for both of my bowel blockages. I didn’t worry either time because I knew I was in good hands.”
December was the last time Haen saw Dr. Ryan. She went to his office for a follow-up appointment.
Though she’s at a moderate to high risk of having another bowel blockage, she’s been doing well this year. She follows up with her regular doctor, eats healthfully and stays active.
“I’m in tune with my body now, so if it happens again, I’ll know to get to the hospital right away,” Haen says.
“This whole experience has made me appreciate my family more, I’ll tell you that,” she adds. “I can’t say enough how thankful I am that Dr. Ryan returned all of my daughter’s phone calls and answered all of her questions. He explained everything very patiently to my family. And his bedside manner is wonderful. It’s good to know there are surgeons out there who care for you.”
A Surgeon’s Perspective
To be a surgeon, compassion is crucial. This is the philosophy of Dr. Daniel J. Farrugia, a fellowship-trained breast surgeon at Centegra Physician Care and the medical director of the Comprehensive Breast Program at Centegra Health System, in McHenry County.
“No matter how routine a problem may seem to a surgeon, it’s life-changing for the patient,” he says. “My goal is to recognize the inner fight in every patient through empathy and understanding. And, by delivering state-of-the-art surgical care, I strive to provide each patient with a sense of peace and diminished suffering.”
Farrugia felt drawn to cancer surgery because he knew that in order to achieve successful outcomes, it was necessary to develop a strong, personal connection with each patient.
He also enjoys how breast surgery, in particular, requires the use of advanced technology for diagnosis and treatment.
“It’s just as much an art as it is a science,” he says.
In addition to completing a fellowship in breast surgical oncology, Farrugia also earned a Ph.D. at the Mayo Clinic College of Medicine. His research concentrated on inherited breast cancer.
“At the time, it hadn’t been long since we discovered that the BRCA1 and BRCA2 genes are responsible for inherited breast cancer, and I was very interested in studying these genes and identifying those mutations that put a woman at risk,” he says. To date, his research has been cited more than 1,200 times in medical literature.
Today, Farrugia focuses on treating breast cancer patients at Centegra. Since surgery remains the mainstay of breast cancer treatment, he’s often the first specialist to meet with a newly diagnosed breast cancer patient. Thus, his job also involves collaborating with other specialists, including those at the Centegra Gavers Breast Center and at the Centegra Sage Cancer Center, to provide patients coordinated treatment.
Genetic testing and counseling, medical and radiation oncology, plastic surgery, nutrition support, rehabilitation services, psychosocial support, financial counseling, art and music therapy, water therapy, and several complementary therapies may be involved.
“In my case, the development of a treatment plan stems from an hour-long conversation with the patient where we develop a personalized treatment plan for the woman’s particular type of cancer. Should surgery come first, or should another form of treatment come first? We also discuss the types of surgery there are,” Farrugia says. “For example, are we doing breast conservation surgery? Can the woman keep her own breast? Or, is a mastectomy with or without reconstruction more appropriate in her case? More importantly, what are the woman’s own preferences and expectations?”
Farrugia and his colleagues also bring new advances to Centegra to give patients access to the best diagnostic technology and breast cancer treatment methods. Recently, the hospital acquired new technology to make breast cancer surgery easier for patients.
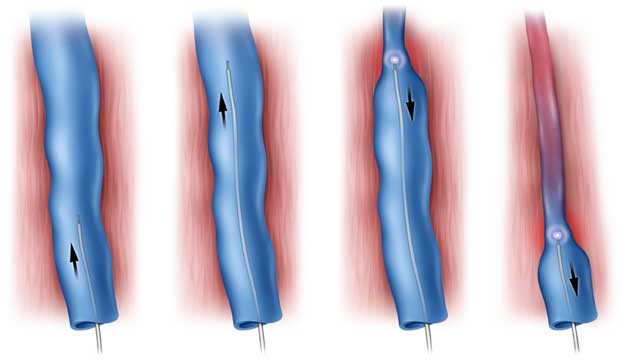
Breast surgeons and radiologists at Centegra now utilize radiofrequency localization tags, a technology that marks the exact location of breast tumors to be removed and improves patient comfort before a lumpectomy surgery. Surgeons can also use this technology for biopsies when it’s unclear whether or not a patient has breast cancer.
“To prepare for lumpectomies in the past, radiologists inserted wires into a woman’s breast to mark the tissue that needed to be excised,” Farrugia says. “However, it had to be done the day of surgery. The woman had to arrive at the hospital several hours before surgery just to have this wire placed. She had to have the wire poking out of her breast, and it was a relatively inaccurate technology.”
Now, radiofrequency localization tags can be used instead of wires. They’re the size of a grain of rice, and a breast radiologist can place them in the center of the lesion up to 30 days before a surgery using either ultrasound or mammogram.
Then, during surgery, the breast surgeon uses a small handheld probe to accurately locate the tag and remove it along with the necessary tissue.
“This provides better accuracy and better patient comfort, and it decreases the hours a woman needs to be in the hospital prior to the surgical procedure,” Farrugia says. “It makes a stressful situation a little bit easier for a woman who’s already going through a difficult time coping with cancer.”
Even though this technology is new at Centegra, Farrugia is already hearing positive feedback from patients.
“I’ve had a few recurring patients who previously underwent localization for lumpectomies using wires, and they cannot believe how much better their experience is when we use this new technology,” he says. “The fact that we can place it on a different day, the fact they don’t have wires coming out of their breast, the fact they don’t have to come to the hospital many hours before their surgery – they thought it was incredible.”
Centegra also recently acquired specialized technology to identify and monitor lymphedema, which is swelling that can be a side effect of surgery.
When a lymph node is sampled during breast cancer treatment, the patient is at an increased risk to develop lymphedema, Farrugia says. With this new technology, he and his colleagues can now monitor for the development of lymphedema months before a physician or patient can detect it themselves.
“It can detect extra fluid in a patient’s arm several months before swelling begins,” he says. “This allows us to address the lymphedema and treat it early before it even becomes an issue. For me, it’s very satisfying to give my patients peace of mind; they go from being concerned about lymphedema to knowing that a plan is already in place to address it before it becomes an issue. The relief is visible on their faces.”
Farrugia’s overall goal is to return each patient to a life that they love living.
“My overarching philosophy is to treat every patient as if I were treating my own family,” he says. “No one deserves less than that.”